
It was New Years Eve, 1997 and life was good. Our home in Palo Alto was filled with people we loved; candles flickered, a fire crackled, and I played DJ, blaring everything from Earth Wind and Fire to Dave Matthews. The small crystals attached to my sweater rubbed against my pregnant belly as my husband twirled me around the makeshift dance floor in our small living room. My due date was April 15th.
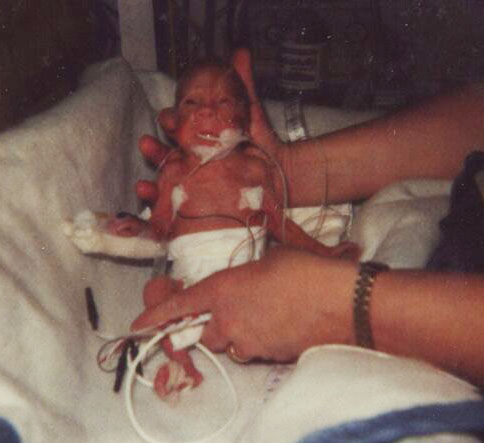
A day or two later, I started feeling weak. Something was wrong. By January 5th, I was rushed to Stanford Hospital in preterm labor and hooked to machines to keep my baby inside. The doctor’s words to us were, “every minute is precious,” “every day will make a difference” and left the room ordering their medical team to do everything possible to keep me pregnant. Less than 24 hours later, I was rushed into emergency C-section surgery. My precious son was taken from my body three months early, weighing only two pounds.
I never noticed the acrid smell of adhesive, until I was wheeled into that NICU, to meet my son. It held down cords, lines, IV’s; the odor permeated the unit. Seventeen years later, I cannot bring myself to wrap a birthday present or holiday gift.
They wheeled me through a sea of bright lights, monitors and machines. All of this technology and equipment was being used to keep my son alive, yet I couldn’t stop seeing it as the enemy.
The next day, we met Dr. Kathy Vandenberg. She was spearheading a program at Stanford Children’s Hospital, called NIDCAP (Newborn Developmental Care & Assessment Program.) She invited us to join this program and explained that NIDCAP supported the physical and caregiving environments of the NICU and enhanced the emotional and physical well being of the premature infant. NIDCAP pioneered an approach to ‘care’ that offered a supportive and nurturing environment within the NICU, and it offered the best chance of protecting the child’s early brain developmental health. We did not hesitate. The answer was yes.

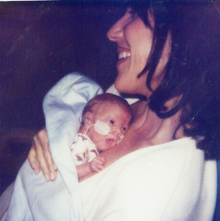
I did not know much at this point, only that my baby needed me and I needed him. Within one day with Dr. Vandenberg’s team of trained NIDCAP professionals, we learned techniques to reduce his stress. Leiseberkhelpthi . For the next three months in the NICU, we were taught how to understand our baby’s voice, through the NIDCAP team. This fragile child had a voice and we learned how to interpret it.
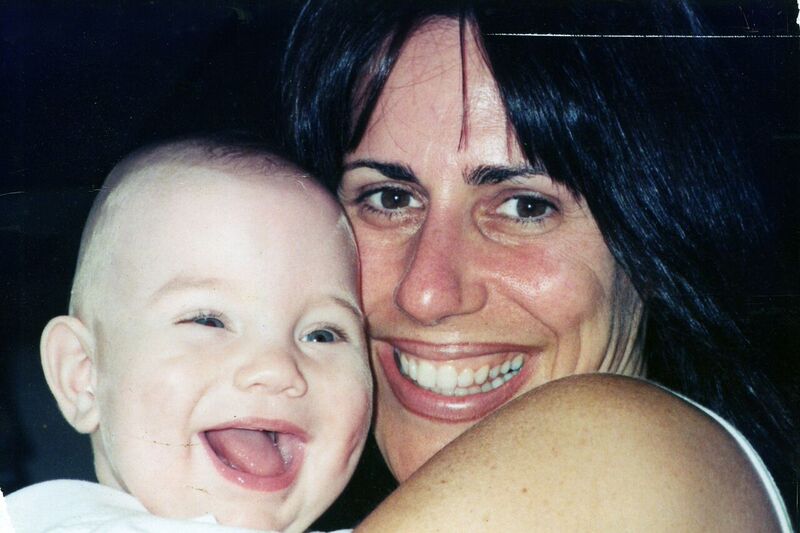
We were involved in every aspect of our son’s care to help create an environment that mimicked the womb. Even within an artificial surrounding, this method would prove to have a huge impact on his brain development and overall health. Our son had less medical complications and was released from the hospital earlier than the babies who did not receive NIDCAP.
No one prepares you when excitement over your pregnancy turns to fear, when faced with pre-term labor, nor remove the agonizing journey of giving birth to a premature infant. No one can remove these traumatic experiences, but NIDCAP walked the path with us and did an outstanding job in educating us in the most efficient ways to support our little guy.

I am grateful to NIDCAP for the skills they taught us.
For the last seventeen years I have watched this program grow and become available in hospitals all over the globe. NIDCAP is now the leading authority in developmental care for high-risk babies born prematurely.
As a former board member, it has been an honor to help promote awareness and raise funds to ensure that NIDCAP is implemented in every hospital throughout the world.

To learn more visit www.nidcap.org.
